Institutional Member Spotlight: Department of Population Health at the NYU School of Medicine
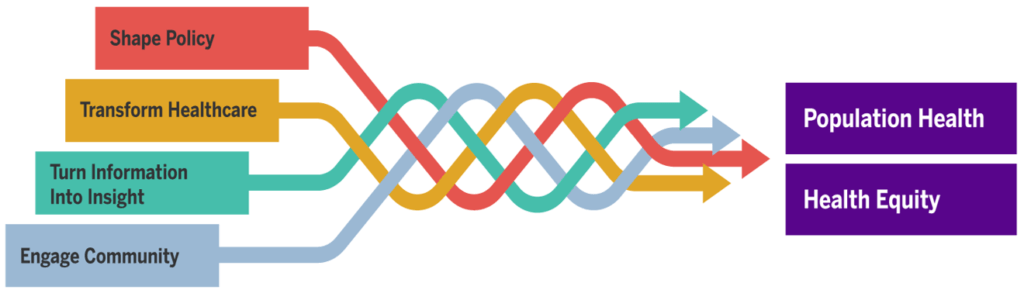
Meghan WolfeThe Department of Population Health at the NYU Grossman School of Medicine was launched in 2012, and in the intervening years has become one of the largest departments of its kind in the country, with more than 100 full-time faculty and 350 staff. With a strong reputation for interdisciplinary research and training, the Department seeks to bridge the divide of medicine and public health to improve the health of populations. It employs four cross-cutting strategies to do so: engaging community, turning information into insight, transforming healthcare delivery, and shaping policy.
The Department’s mission is to improve population health for all while simultaneously reducing health inequities. Faculty engage in research on diverse topics, but the following are some key areas of focus:
- Reducing health and environmental disparities among underserved and historically marginalized populations. The Department also explicitly examines how public policy and the built environment impact heath and the choices people make.
- Combating the opioid epidemic. The Center for Opioid Epidemiology and Policy, recently launched, examines the impact of state policies such as the monitoring of opioid prescribing and marijuana legalization. Department faculty are also creating new models to identify and link patients to addiction care, as well as investigating opioid alternatives through trials reaching high-risk populations.
- Redesigning healthcare and improving patient outcomes by fostering a learning healthcare system.
- Early childhood development initiatives, such as the ParentCorps program.
- Educating future leaders in population health through training programs for medical and other graduate students, including PhD programs in epidemiology, biostatistics, and most recently, population health.
Leading research that spurs action and impact is at the core of the Department’s work. Numerous research projects, population health initiatives, and community-centered programs have demonstrated the Department’s commitment to improving health in New York City and beyond. Here’s a closer look at the impact of three initiatives:
Community Health Worker Models
The NYU-CUNY Prevention Resource Center is one of 25 CDC-funded academic centers in the United States that study how people and communities can avoid or counter risks for chronic illnesses. One of the major areas of impact that the Center has led is developing and implementing community health worker (CHW) models. For example, one ongoing study bridges CHWs, the delivery system’s EHR, and a large Medicaid managed care payer to deliver improved hypertension control among South Asian patients—who have disproportionately high rates of cardiovascular disease, diabetes, and obesity while facing numerous cultural and social barriers to accessing healthcare. Study participants who completed this intervention experienced a greater reduction in both systolic and diastolic blood pressure, and blood pressure control improved more than 30 percent. The EHR component of the study allowed primary care practices to better identify hypertensive patients to bring them back to the clinic, while CHWs built trust with patients and served as a bridge between communities and health systems.
In other research, led by the Department’s Division of Health and Behavior, community-engaged interventions in barbershops and churches have proven effective in addressing cardiovascular health improvement and cancer prevention in African American populations at elevated risk for related outcomes.
ParentCorps
ParentCorps is a family-centered intervention that aims to help parents and early childhood teachers create environments in which children thrive. Partnering with school-based leaders, a team of diverse researchers, clinicians, and educators delivers ParentCorps as an enhancement to pre-K in historically disinvested neighborhoods. The program centers racial equity and the voices of people of color throughout all aspects of strategic planning, resource allocation, implementation, and evaluation.
ParentCorps began in 2000 with a pilot program in New York City, involving 40 families in one public school in central Harlem. By 2019, in partnership with NYC’s Department of Education Division of Early Childhood Education as part of Pre-K for All, 54 pre-K programs are implementing ParentCorps, serving more than 3,000 children and families annually. For more information, read more about the evaluation of ParentCorps and the impact of the program.
City Health Dashboard
The City Health Dashboard is a tool for policymakers and other decision-makers to assess health, the factors that shape it, and the drivers of health equity in their communities.
The City Health Dashboard offers data on 37 measures for the 500 largest U.S. cities (those with populations of about 66,000 or more), representing approximately one-third of the U.S. population. The measures address health outcomes (including life expectancy), social and economic factors (e.g., graduation rates, housing costs), health behaviors, the physical environment, and clinical care. The Dashboard site also provides success stories and blog posts about how the data is being used at the local level to improve the health of city residents.
Marc Gourevitch, MD, MPH is chair of the Department of Population Health at the NYU Grossman School of Medicine. To read more about the Department’s work, visit its website and check out this article, Advancing Population Health at Academic Medical Centers: A Case Study and Framework for an Emerging Field.





All comments will be reviewed and posted if substantive and of general interest to IAPHS readers.