In nine podcast episodes, David Kindig MD, PhD, a population health thought leader, is interviewed by Sanne Magnan MD, PhD about his 50 year population health scholarly and policy journey, including many stories, anecdotes and take-aways.
In nine podcasts, David Kindig MD, PhD, a population health thought leader, is interviewed by Sanne Magnan MD, PhD about his 50 year population health scholarly and policy journey, including many stories, anecdotes and take-aways. Dr. Kindig is an Emeritus Professor of Population Health Sciences at the University of Wisconsin-Madison School of Medicine and Public Health. He is an Interdisciplinary Association for Population Health Science (IAPHS) founding Board Member and the Founding/Emeritus Co-Chair of the National Academies of Sciences, Engineering and Medicine (NASEM) Roundtable (RT) on Population Heath Improvement. Dr. Magnan is a Senior Fellow at HealthPartners Institute, a previous co-chair of the NASEM RT on Population Health Improvement, previous IAPHS Board member, and the Minnesota Commissioner of Health from 2007-2010.
Five articles on population health that Kindig says are the most important to read of his writings:
- Kindig D. 2015. What Are We Talking About When We Talk About Population Health? Health Affairs blog April 6. 1377/forefront.20150406.046151
- Kindig D. 2015. From Health Determinant Benchmarks to Health Investment Benchmarks. Prev Chronic Dis 12:150010. DOI: http://dx.doi.org/10.5888/pcd12.150010
- Kindig DA, Isham G. 2014. Population Health Improvement: A Community Health Business Model That Engages Partners in All Sectors. Front in Health Serv Manage 30(4):3-20. This paper won the 2014 American College of Healthcare Executives (ACHE) Dean Conley Article of the Year Award.
- Kindig D. 2015. Can There Be Political Common Ground for Improving Population Health? Milbank Q 93(1):24–27.
- Kindig D. 2017. Population Health Equity: Rate and Burden, Race and Class. JAMA 317(5):467-468.
- Advances in methodology and data quality have brought us closer to understanding how to balance the multiple determinants of health.
- Using this information, set per-capita investment benchmarks across determinants, with a sharp focus on raising the mean and closing gaps/improving equity.
- Spend less in wasteful, unneeded health care and invest more in social determinants, especially with disadvantaged children.
- Financial formula model(s) like mortgage interest deduction or crop subsidies are devised and implemented to drive these rebalanced investments.
- There are robust multisectoral health outcome trusts or community business model partnerships with adequate core funding to be effective.
- Political and ideological common ground and social solidarity are built to make these five previous points sustainable.
Environment
- What happens outside the clinic is as or more important than what happens inside, a concept not widely embraced in health care in the 1960’s and 1970’s.
Population Health – general
- Everything Kindig has done in population health research and advocacy has its origins in the Evans-Stoddart 1990 paper “Producing Health, Consuming Health Care” – -i.e., it takes more than disease management and more than medical care to produce health.
- Population health needs a clear outcome measurement definition – -not enough to be just a study of determinants. This led to the initial “health adjusted life expectancy definition.”
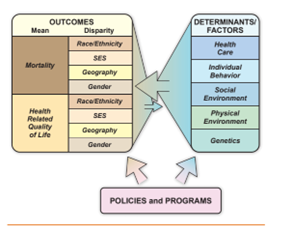
- Kindig defined population health as a health outcome concept, some combination of mortality and morbidity/functional status as well as disparity or equity differences across subgroups.
- It implicitly recognizes that such outcomes are produced by multiple determinants, not just medical care.
- Population health management refers to health outcomes of enrolled clinical populations, but often limited to health care quality.
- There is a beginning appreciation in the first decade of this century that population health is more than health care, yet the full appreciation for the social determinants is slow in coming. It is hard for most to understand how the social determinants “get under the skin”.
Incentives
- Financial incentives are critical but can be overdone such as fee-for-service, and the idea of capitation changes the incentive orientation.
- “Why not financial incentives for health outcomes instead of simply health care/services?”
- Grants are not enough for major change. For something so major, ongoing formulas like crop subsidies and graduate medical funding (GME) funding are needed.
Pay for Population Health
- The fundamental assertion of Kindig’s book Purchasing Population Health: Paying for Results is that population health improvement needs appropriate financial incentives designed for this outcome.
- Measures, financial incentives, coordination across sectors – – important concepts are key challenges for a pay for population health model, as well as the importance of a common language and understanding across disciplines.
- Complex ideas such as paying for population health take time to gain broad understanding.
Investments
- An “investment balancing function” across determinants is critical – one that encompasses fairness.
- One key take-away continues to surface – the challenge of balancing investments across determinants.
- We need much more research on relative cost effectiveness, so cross sectoral investment benchmarks can be set.
- There is promise in community multisectoral partnerships including business as well as government, non-profits like United Way, health care and public health, but need core resources to function effectively.
County Health Rankings Model
- The County Health Rankings model – three main points:
- Clearly derived from original Evans and Stoddart 1990 and 2003 articles
- Separated outcomes from determinants
- Needed to estimate weights in order to rank…e.g., 20% health care weight -driving home that more than health care is needed
- In the second decade, new disseminations were needed for population health concepts. A blog and the Roundtable for Population Health Improvement associated with the National Academies for Sciences, Engineering and Medicine (NASEM) were created, which reached a wider, diverse audience.
Equity
- Population health equity is crucial and complicated.
- There are twin goals of population health – raise the mean; close the gaps. Having equal but very low outcomes is not acceptable; it’s not equitable – not fair and just.
- The balance of outcomes we desire reflects value choices for individuals and jurisdictions.
- No single group characteristic or health outcome represents the whole picture of health inequalities in a population.
- Addressing racism is central and essential to addressing black, indigenous, Asian and Latinx inequities, but there is a counterpart history of poor white classism that persists today as well. It is not well understood and needs policy attention as well.
- Absolute numbers are as important as high rates. Can understanding burden and rate – can this lead to more common ground – e.g., black/white, urban/ rural – on equity policy and investment?
Miscellaneous
- Excessive health care expenditures are the perfect storm of American culture… wanting more of everything now, greed in medicine, fascination with technology, etc. As Starr said in the Social Transformation of Medicine, professional power gets medical care expansion without controls.
EPISODES:
Release date: September 28, 2022
https://sickindividualssickpopulations.blubrry.net/2022/09/28/1-once-upon-a-time-with-david-kindig/
Population Health: the Unfinished Journey with David Kindig
Episode 1: Once Upon A TimeDave discusses his South Bronx roots of seeing “health” vs only healthcare, and how an unfavorable, chance encounter with the Chair of Pediatrics changed his career forever.
References:
Kindig DA. 1992. The Health Care System Should Produce Health. On Wisconsin September/October. p.25.
Evans RG, Stoddart GL. 1990. Producing Health, Consuming Health Care. Soc Sci Med 31(12):1347-1363.
We thank the staff of IAPHS for the production and support of this podcast.
Podcast #2
The Story Behind the Book Purchasing Population Health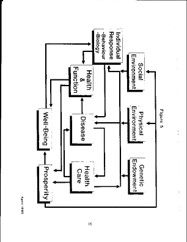
Evans and Stoddart 1990 Field Model – Used with permission
Evans RG, Stoddart GL. 1990. Producing Health, Consuming Health Care. Soc Sci Med 31(12):1347-1363.Dave explores with Sanne the seminal, Canadian influence and how his sabbatical intellectual paralysis in York England almost resulted in no book. He reminds us of the only italicized sentence in the seminal Evans and Stoddart 1990 paper: “A society that spends so much on health care that it cannot or will not spend adequately on other health enhancing activities may actually be reducing the health of its population.”
Kindig DA. 1997. Purchasing Population Health: Paying for Results
TABLE OF CONTENTS
Chapter 1. Purchasing Population Health: A Vision
Chapter 2. Taking Our Temperature: How Healthy Are We?
Chapter 3. The High Cost of Health Care: Are We Getting the Most for Our Money?
Chapter 4. Measuring Health Outcomes
Chapter 5. The Multiple Determinants of Health
Chapter 6. Can Rationing Be Rational? Balancing the Determinants of Health
Chapter 7. Managing Boundaries
Chapter 8. Different Populations, Different Needs?
Chapter 9. Making It Happen
Chapter 10. The Case for Action, The Price of InertiaReferences for the Podcast:
1. Evans RG, Stoddart GL. 1990. Producing Health, Consuming Health Care. Soc Sci Med 31(12):1347-1363.
2. Evans RG, Barer ML, Marmor TR, editors. 1994. Why Are Some People Healthy and Others Not? The Determinants of Health of Populations. New York: Aldine de Gruyter.
3. Kindig DA. 1997. Purchasing Population Health: Paying for Results. University of Michigan Press: Ann Arbor, MI.
Podcast #3
What is Population Health?Dave discusses the evolution of his definition of population health to his most cited 2003 paper and clarifies ongoing confusion with the terms “public health” and “population health management”.
References:
- Kindig D, Stoddart G. 2003. What is Population Health? Am J of Public Health 93(3): 380-383.
- Kindig D. 2015. What Are We Talking About When We Talk About Population Health? Health Affairs Blog April 6. 1377/forefront.20150406.046151
- https://www.nationalacademies.org/our-work/roundtable-on-population-health-improvement
Podcast #4
The Lonely YearsSanne encourages Dave to explain why he describes this period of slow up-take as “lonely,” despite several major presentations, and how a rejected paper returned to prominence.
References:
- Kindig DA. 1999. Beyond Health Services Research (Association for Health Services Research (AHSR) Presidential Speech). Health Services Research 34(1):205-214.
- Kindig DA. 2006. A Pay-for-Population Health Performance System. JAMA 296(21):2611-2613.
- Kindig DA. 2007. Understanding Population Health Terminology. Milbank Q 85(1):139-161.
Podcast #5
Picking Up Steam 2006-2014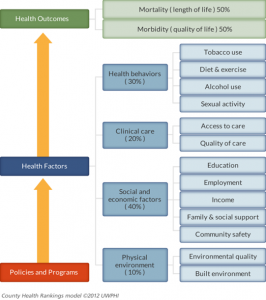
County Health Rankings Model Dave tells us about how the population health idea began to catch on, in scholarship as well as in the County Health Rankings, Federal Medicare and Medicaid. The momentum continued in his blog and the founding of the Institute of Medicine Roundtable on Population Health Improvement …saying to Robert Wood Johnson “…they couldn’t say no”.
References:
- Kindig DA, Asada Y, Booske B. 2008. A Population Health Framework for Setting National and State Health Goals. JAMA 299(17):2081-2083.
- Kindig D. 2008. Beyond the Triple Aim: Integrating the Nonmedical Sectors. Health Affairs Blog May 19. https://www.healthaffairs.org/do/10.1377/forefront.20080519.000393/full/
- Peppard PE, Kindig DA, Dranger E, Jovaag A, Remington PL. 2008. Ranking Community Health Status to Stimulate Discussion of Local Public Health Issues: The Wisconsin County Health Rankings. Am J Public Health 98(2):209-212.
- Kindig DA, Booske BC, Remington PL. 2010. Mobilizing Action Toward Community Health (MATCH): Metrics, Incentives, and Partnerships for Population Health. Prev Chronic Dis 7(4). https://www.cdc.gov/pcd/collections/pdf/PCD_MATCH_2010_web.pdf
- Kindig D. Feb 3, 2017. https://iaphs.org/improving-population-health-continuing-journey/
- Kindig D. 2011-2014. Improving Population Health: Ideas and Action. Electronic blog collection (43 posts). https://uwphi.pophealth.wisc.edu/wp-content/uploads/sites/316/2018/03/blog-collection-final-2014-04-05.pdf
7. The Roundtable on Population Health Improvement. National Academies of Sciences, Engineering and Medicine. https://www.nationalacademies.org/our-work/roundtable-on-population-health-improvement
Podcast #6
It’s All About the MoneySanne probes Dave’s efforts to promote rebalancing to upstream investments, calling in 2015 for per capita investment benchmarks for all determinants. He discusses the potential but yet unrealized promise of ACO Shared Savings, the Hospital Community Benefit IRS requirement, and local health outcome trusts.
References:
- Kindig DA, Isham G. 2014. Population Health Improvement: A Community Health Business Model That Engages Partners in All Sectors. Front Health Serv Manage 30(4):3-20.
- Rosenbaum S, Kindig DA, Bao J, Byrnes M, O’Laughlin C. 2015. The Value of the Nonprofit Hospital Tax Exemption Was $24.6 Billion in 2011. Health Affairs 34(7):1225-1233.
https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.1424 - Bakken E, Kindig DA. 2012. Is Hospital Community Benefit Charity Care? Wisconsin Medical Journal 111(5):215-219.
- Kindig D. 2016. To Launch and Sustain Local Health Outcome Trusts, Focus On ‘Backbone Resources’. Health Affairs Blog February 10. https://www.healthaffairs.org/do/10.1377/forefront.20160210.053102/full/
- Kindig D. 2015. From Health Determinant Benchmarks to Health Investment Benchmarks. Chronic Dis 12:150010. DOI: http://dx.doi.org/10.5888/pcd12.150010
- Kindig DA, Milstein B. 2018. A Balanced Investment Portfolio for Equitable Health and Well-Being Is an Imperative, and Within Reach. Health Affairs 37(4):579-584. https://doi.org/10.1377/hlthaff.2017.1463
Podcast #7
Population Health Equity: Finding Common GroundDave explains his provocative and contrarian statement: “The effort to reduce health disparities is hindered by viewing health equity only in terms of racial inequities.” And he argues for seeing inequities through multiple lenses to find common ground.
References:
- Kindig DA. 2015. Can There Be Political Common Ground for Improving Population Health? Milbank Q 93(1):24–27.
- Haidt J. 2012. The Righteous Mind: Why Good People Are Divided by Politics and Religion. New York, NY. Pantheon Books.
- Isenberg N. 2016. White Trash: the 400-Year Untold History of Class in America. New York, New York. Viking.
- Kindig D. 2017. Population Health Equity: Rate and Burden, Race and Class. JAMA 317(5):467-468.
- Kindig DA. 2020. Using Uncommon Data to Promote Common Ground for Reducing Infant Mortality. Milbank Q 98(1):18–21.
Podcast #8
Population Health Equity: Crucial and ComplicatedSanne asks Dave why a paper he worked on for three years “Thinking Clearly, Speaking Frankly about Health Equity” was never published…and whether the many complications of population health equity can detract from crucial action.
****Attach the Unpublished Draft Kindig Paper “Thinking Clearly and Speaking Frankly about Health Equity: Good and Fair Population Health”
References:
- Asada Y, Whipp A, Kindig D, Billard B, Rudolph B. 2014. Inequalities in Multiple Health Outcomes by Education, Sex, and Race in 93 US Counties: Why We Should Measure Them All. Int J Equity Health 13:47. https://doi.org/10.1186/1475-9276-13-47
- Kindig D, Lardinois N, Chatterjee D. 2016. Can States Simultaneously Improve Health Outcomes and Reduce Health Outcome Disparities? Prev Chronic Dis 13:160126. http://dx.doi.org/10.5888/pcd13.160126
- Kindig D, Lardinois N, Asada Y, Mullahy J. 2018. Considering Mean and Inequality Health Outcomes Together: the Population Health Performance Index. Int J Equity Health 17:25. DOI 10.1186/s12939-018-0731-2.
- Givens ML, Kindig D, Inzeo PT, Faust V. 2018. Power: The Most Fundamental Cause of Health Inequity? Health Affairs Blog Feb 1. https://www.healthaffairs.org/do/10.1377/forefront.20180129.731387/full/
- Gundersen G, Pray L. 2009. Leading causes of life: five fundamentals to change the way you live your life. Abingdon Press, Nashville Tennessee.
Podcast #9
Looking Ahead in an Unfinished JourneyReferences:
- Kindig DA. 2015. Can There Be Political Common Ground for Improving Population Health? Milbank Q 93(1):24–27.
- Kindig DA. 2007. Understanding Population Health Terminology. Milbank Q 85(1):139-161.
- Kindig D, Nobles J, Zidan M. 2018. Meeting the Institute of Medicine’s 2030 US Life Expectancy Target. Am J Public Health108(1):87-92.
- McCullough JM, Speer M, Magnan S, Fielding JE, Kindig D, Teutsch SM. 2020. Reduction in US Health Care Spending Required to Meet the Institute of Medicine’s 2030 Target. Am J Public Health 110(12):1735-1740.
- Hughes-Cromwick P, Kindig D, Magnan S, Gourevitch M, Teutsch 2021. The Reallocationists Versus the Direct Allocationists. Health Affairs Forefront. August 6. https://www.healthaffairs.org/do/10.1377/forefront.20210729.55316
- Kindig D. 2022. The Promise of Population Health: A Scenario for the Next Two Decades. NAM Perspectives. Commentary, National Academy of Medicine. Washington, DC. https://doi.org/10.31478/202203a
- Kindig D. 2020. A Population Health Boot Camp. https://iaphs.org/a-population-health-boot-camp/
- Wagstaff A. 2002. Inequality aversion, health inequalities and health achievement. J Health Econ 21(4):627–41. https://pubmed.ncbi.nlm.nih.gov/12146594/